Technical progress of interventional stent coating
The drug-eluting stent (DES), which came out in 2000, successfully solved the problem of restenosis of the previous bare metal stent (BMS), and became one of the milestones in the history of interventional treatment of coronary heart disease. The permanent polymer coating on the surface of traditional DES can cause chronic inflammation of the blood vessel wall and become an important cause of late stent thrombosis (ST). The subsequently developed degradable polymer-coated stents usually use polylactic acid as the drug-carrying coating. After the drug is completely released, the coating can be completely degraded in 6-10 months, which minimizes the impact of the coating on the blood vessel wall. Reduce the risk of advanced stent thrombosis.
However, the current development of DES has entered a bottleneck stage. Whether it is the improvement of the stent platform, stent coating or anti-proliferative drugs, the effect on the efficacy of the stent has been relatively small, and the safety of the stent is undoubtedly improved when the efficacy of various stents is equivalent It is a good choice. At this point, stent manufacturers have made many attempts. Polymer-free coating technology, asymmetric coating, surface notch technology, eG™ technology, and Ti-O film all show the innovative capabilities of stent manufacturers.
- Polymer-free coating technology
In order to control the release of drugs, the traditional DES drug-loading coating materials use high-molecular polymer materials. These coating materials can stimulate the stent and its adjacent segment arteries to produce persistent oxidative stress and inflammatory hypersensitivity, which may It causes damage to the endothelialization process and vascular endothelial function of the stent, and can lead to the occurrence of poor stent adhesion in the late stage. These factors may be the susceptibility factors of stent thrombosis in the late stage of DES, especially the very late stage. The polymer-free coating technology further ensures safety, avoids the introduction of ineffective foreign bodies, facilitates advanced vascular endothelialization, and reduces the probability of thrombosis. For example, Zilver PTX peripheral drug-eluting stent.
- Asymmetric coating technology
In previous studies, there was no significant difference in the total thrombosis rate in the first year after DES and BMS implantation. However, after 1 year, the incidence of very late stent thrombosis in DES was significantly higher than that of BMS, which may be compared with traditional DES drug delivery. Coating design related ①The drug-loaded coating of traditional DES is a symmetrical design, that is, there are drug coatings on the side of the vessel wall and the inner side of the vessel lumen of the stent. The anti-proliferative drugs gradually released from the coating on the side of the stent wall can inhibit the excessive proliferation of smooth muscle cells in the vessel wall, thereby significantly reducing the incidence of restenosis in the stent; however, the anti-proliferative drugs gradually released from the coating on the inner side of the vessel lumen are not only The lack of beneficial biological effects instead inhibits the endothelialization of the stent and damages the endothelial function of the stent and its adjacent segments. ②Traditional DES drug-loaded coating materials are all biodegradable polymers, which persist even after the drug is completely released. These factors may be the susceptibility factors of stent thrombosis in the late stage of DES, especially the very late stage. Therefore, the improvement of coating design may overcome the inherent shortcomings of traditional DES.
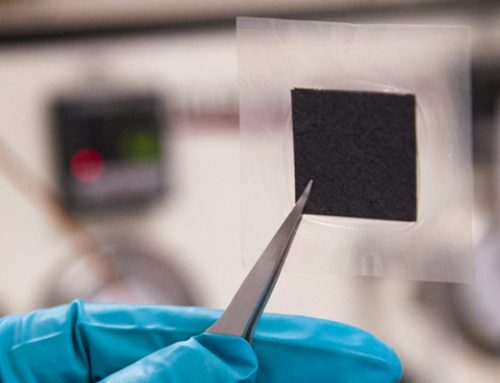
The coating design of the new asymmetric and degradable coating DES is asymmetric, that is, the stent is only coated with a degradable polymer coating containing anti-proliferative drugs on the side of the vessel wall, and there is no drug coating on the inside of the vessel lumen. It can avoid endothelial toxicity caused by the release of drugs inside the vascular cavity.
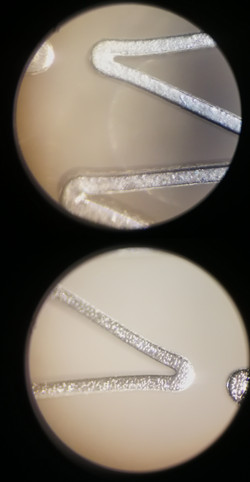
- Surface groove technology
Different from traditional drug-eluting stents, the coating technology with grooves on the surface has a lower amount of drug and polymer. That is, the drug coating is only stored in the grooves on the outer surface of the stent. After the stent is expanded, the drug only moves toward the vessel wall. Release, and the drug release rate is effectively controlled by the polymer, so that a smaller amount of the drug can maintain a longer effective therapeutic concentration in the blood vessel. For example, Firehawk® coronary rapamycin targeted eluting stent system.
- eG™ technology
With biodegradable drug coating and electronic grafting technology (electrografting, eG™) inert coating technology, it solves the problem of coating cracking after conventional stents are crimped or expanded, and reduces endothelialization delay caused by coating cracks. Ensure product effectiveness and long-term safety. Clinical studies have shown that after the biodegradable coating is degraded, eG™ can promote the process of endothelialization after stent implantation. For example, BuMA™ drug-eluting stent.
- Ti-O film
In recent years, Chinese scientists have discovered that titanium oxide (Ti-O) with an n-type semiconductor and rutile structure has a significant inhibitory effect on the conceptual changes in the adsorption of fibrinogen and the activation of platelets. The prepared titanium oxide film can promote endothelial cells The function of growth and vascular intimal repair. At the same time, the design of the coating is based on the sequential functional layer of “early anti-stenosis and late anti-thrombosis”. The early degradable polymer drug coating can effectively inhibit the occurrence of stenosis, and the titanium oxide film can promote blood vessels after the release of the late drug coating. Repair of the inner membrane. At the same time, because the titanium oxide film has a long-term anticoagulant effect, it can effectively inhibit the occurrence of late thrombosis in the stent. For example, Helios drug stent.
The occurrence of complications after intraluminal stent implantation is the result of many factors. The idea of using metal stent surface modification exogenous methods to inhibit restenosis has proved feasible in practice. From the design idea of stent coating: how to organically combine the inert coating with the active coating, on the one hand to play the shielding function of the inert coating, and on the other hand to play the biocompatibility advantage of the active coating, A direction for the future development of stent coating.
Source: Xinmai Company’s internal R&D personnel

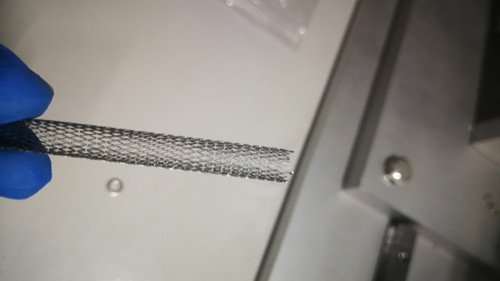
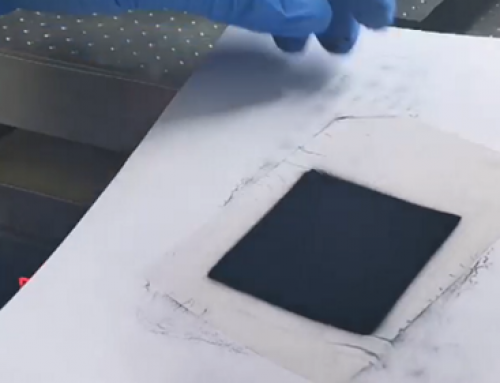
The ultrasonic coating system can be used to spray the anti-restenosis drug-eluting polymer solution onto the implantable stent. He has expertise in spraying hundreds of different medical grade polymer chemicals. Ultrasonic nozzles have advantages in spraying complex stent geometries to ensure coverage of all pole surfaces of the stent. The soft atomized spray can adhere well to the surface, and the morphological characteristics of the coating can be adjusted by modifying the process parameters. High-pressure nozzles cannot apply the coating evenly like ultrasonic coating systems. Compared with dip coating, the coating applied by ultrasonic is much thinner, saving spray material. Because the ultrasonic nozzle is rarely blocked, the spray quality will not decrease over time.
Technical progress of interventional stent coating – Cheersonic